Afatinib Drug Side Effects, Mechanism of Action & More
Hasan
06 Jan, 2025
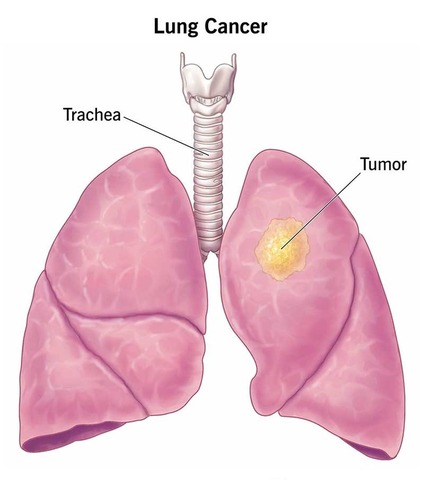
Afatinib (Afanix) is approved as a first-line treatment for metastatic non-small cell lung cancer (NSCLC) in patients with tumors exhibiting EGFR exon 19 deletions or exon 21 (L858R) substitution mutations, confirmed by an FDA-approved test.
Afanix 40 mg tablet: Each film coated tablet contains Afatinib Dimaleate INN equivalent to Afatinib 40 mg.
Table of Contents
Side Effects
Most common side effects (>_20%) are diarrhea, rash/dermatitis acneiform, stomatitis, paronychia, dry skin, decreased appetite and pruritus.
Mechanism of Action
Afatinib functions by covalently binding to the kinase domains of EGFR (ErbB1), HER2 (ErbB2), and HER4 (ErbB4), leading to the irreversible inhibition of tyrosine kinase autophosphorylation. This process ultimately leads to the downregulation of ErbB signaling.
In various experiments, Afatinib drug exhibited the ability to inhibit autophosphorylation and in vitro proliferation of cell lines expressing wild-type EGFR. It also demonstrated effectiveness against cell lines expressing specific EGFR exon 19 deletion mutations, exon 21 L858R mutations, and those with a secondary T790M mutation. Moreover, Afatinib proved to inhibit the in vitro proliferation of cell lines that overexpress HER2.
The therapeutic impact of Afatinib was evident in nude mice implanted with tumors, including those overexpressing wild-type EGFR, HER2, or in an EGFR L858R/T790M double mutant model. In these cases, treatment with Afatinib resulted in the inhibition of tumor growth.
Cardiac Electrophysiology
The effect of multiple doses of Afatinib drug (50 mg once daily) on the QTc interval was evaluated in an open-label, single-arm study in patients with relapsed or refractory solid tumors. No large changes in the mean QTc interval (i.e., >20 ms) were detected.
Absorption and Distribution
Upon oral administration of Afatinib tablets, it takes 2 to 5 hours to reach peak plasma concentrations (Tmax). The Maximum concentration (Cmax) and the area under the concentration-time curve from time zero to infinity (AUC0-∞) values exhibited a slightly greater than dose-proportional increase within the 20 to 50 mg dosage range.
The geometric mean relative bioavailability of 20 mg Afatinib tablets was found to be 92% when compared to an oral solution. In terms of in vitro binding, Afatinib binds to approximately 95% of human plasma proteins. The presence of a high-fat meal resulted in a 50% reduction in Cmax and a 39% decrease in AUC0-∞ compared to the fasted condition.
Metabolism and Elimination
The predominant circulating metabolites of Afatinib are covalent adducts with proteins, with minimal enzymatic metabolism observed. In humans, the primary route of Afatinib excretion is through feces (85%), with 4% excreted in urine following a single oral dose of [14C]-labeled Afatinib solution. The parent compound constitutes 88% of the recovered dose.
After repeated dosing in cancer patients, Afatinib exhibits an elimination half-life of 37 hours. Steady-state plasma concentrations are attained within 8 days of repeat dosing, leading to an accumulation of 2.8-fold for AUC and 2.1-fold for Cmax.
Specific populations
Renal Impairment
In patients with mild (CLcr 60-89 mL/min) and moderate (CLcr 30-59 mL/min) renal impairment, the median trough Afatinib plasma concentrations were 27% and 85% higher, respectively, compared to those with normal renal function (CLcr ≥ 90 mL/min). Afatinib has not been investigated in patients with severe renal impairment (CLcr < 30 mL/min).
Hepatic Impairment
Afatinib is primarily eliminated through biliary/fecal excretion. Mild (Child Pugh A) or moderate (Child Pugh B) hepatic impairment demonstrated no impact on Afatinib exposure after a single dose. The effects in subjects with severe hepatic dysfunction (Child Pugh C) have not been explored.
Body Weight, Gender, Age, and Race
According to population pharmacokinetic analysis, factors such as weight, gender, age, and race do not exert a clinically significant influence on Afatinib exposure.
Drug Interactions
Exploring the Impact of Ritonavir on Afatinib Pharmacokinetics:
In a study involving healthy subjects, the influence of ritonavir dosing time in relation to a single oral dose of 40 mg Afatinib was investigated. When ritonavir (200 mg twice daily for 3 days) was administered 6 hours after Afatinib, the relative bioavailability for AUC0-∞ and Cmax of Afatinib increased by 119% and 104%, respectively. Similarly, when ritonavir was administered 1 hour before a 20 mg single dose of Afatinib, exposure to Afatinib rose by 48% for AUC0-∞ and 39% for Cmax.
In contrast, pre-treatment with rifampicin, a potent P-gp inducer (600 mg once daily for 7 days), led to a decrease in plasma exposure to Afatinib by 34% (AUC0-∞) and 22% (Cmax). These findings highlight the dynamic interactions between ritonavir, rifampicin, and Afatinib, offering insights into optimizing their co-administration for therapeutic efficacy.
P-glycoprotein (P-gp): Based on in vitro data, afatinib drug is a substrate and an inhibitor of P-gp.
Breast Cancer Resistance Protein (BCRP): Based on in vitro data, afatinib is a substrate and an inhibitor of the transporter BCRP.
CYP450 Enzymes: Afatinib has been found to neither inhibit nor induce CYP450 enzymes, including CYP1A2, 2B6, 2C8, 2C9, 2C19, and 3A4, in cultured primary human hepatocytes. This indicates that Afatinib is unlikely to interfere with the metabolism of other drugs that serve as substrates for CYP450 enzymes. These findings contribute to the understanding of Afatinib’s compatibility with co-administered medications, assuring minimal impact on their metabolic pathways.
Dosage & Administration
The recommended dose of Afatinib drug is 40 mg orally once daily until disease progression or no longer tolerated by the patient. Afatinib should be taken at least 1 hour before or 2 hours after a meal. Patients should not take a missed dose within 12 hours of the next dose.
Modification Dosage
- In case of any drug-related side effects, including NCI CTCAE Grade 3 or higher, Grade 2 or higher diarrhea persisting for 2 or more consecutive days despite anti-diarrheal medication, Grade 2 cutaneous reactions lasting over 7 days, or Grade 2 or higher renal dysfunction, it is recommended to withhold Afatinib drug.
- Resume treatment once the adverse reaction fully resolves, returns to baseline, or improves to Grade 1.
- When reinstating Afatinib, consider a reduced dose, specifically 10 mg per day less than the dose at which the adverse reaction occurred.
- Permanently discontinue Afatinib for severe conditions such as life-threatening bullous, blistering, or exfoliative skin lesions, confirmed interstitial lung disease (ILD), severe drug-induced hepatic impairment, persistent ulcerative keratitis, symptomatic left ventricular dysfunction, or severe/intolerable side effects occurring at a 20 mg per day dose.
These guidelines aim to ensure patient safety and optimize the management of adverse events during Afatinib treatment.
Use in Specific Populations
Pregnancy Category D
Due to its mechanism of action, Afatinib has the potential to cause fetal harm if administered to pregnant women. In animal studies, Afatinib demonstrated embryotoxicity, leading to late gestational stage abortions in rabbits at doses of 5 mg/kg or higher (approximately 0.2 times the exposure by AUC at the recommended human dose of 40 mg daily). Patients should be informed of the potential risk to the fetus if this drug is used during pregnancy or if they become pregnant while taking it.
Nursing Mothers
The presence of Afatinib in human milk is currently unknown. Studies in lactating rats revealed concentrations in milk 80-150 times higher than those in plasma within 1 to 6 hours post-administration. Considering the potential for serious side effects in nursing infants due to Afatinib and the common occurrence of drugs in human milk, a decision should be carefully considered. Mothers should weigh the importance of the drug to their health against the potential risks, leading to a choice between discontinuing nursing or discontinuing the Afatinib drug.
Pediatric Use
The safety and effectiveness of Afatinib in pediatric patients have not been established.
Geriatric Use
Among the 3865 patients included in clinical studies of Afatinib, 32% were aged 65 and older, with 7% being 75 years and older. There were no discernible differences in safety between patients aged 65 and over and those younger. In a subset of 345 patients, 39% were 65 or older, and 4% were 75 or older, with no overall disparities in effectiveness noted between patients aged 65 and older and their younger counterparts.
Reproductive Potential
Patients should receive counseling on pregnancy planning and prevention while undergoing treatment with Afatinib drug. Female patients of reproductive potential are advised to use highly effective contraception throughout the duration of Afatinib treatment and for at least 2 weeks following the last dose. Patients are instructed to promptly contact their healthcare provider if they become pregnant or suspect pregnancy while taking Afatinib drug.
Overdose
Two healthy adolescents were reported to have ingested 360 mg of Afatinib each, as part of a mixed-drug ingestion. This led to symptoms such as nausea, vomiting, asthenia, dizziness, headache, abdominal pain, and elevated amylase (less than 1.5 times the upper limit of normal [ULN]). Fortunately, both subjects experienced recovery from these symptoms.
Storage Conditions
Store in a cool and dry place, away from light. Keep out of the reach of children.
